SINGAPORE – More care options for seniors and greater support for mental wellness are among the changes Singapore’s healthcare sector will see in 2026.
This follows developments such as the launch of a new government agency to lead Singapore’s pandemic preparedness efforts, and the continued expansion of the country’s healthcare capacity in 2025.
The Straits Times highlights what to look out for in 2026, as well as key developments in the past year.
In 2026, Singapore is projected to join other countries such as Japan and South Korea in becoming a super-aged society, where at least 21 per cent of the population are aged 65 or older.

In 2026, Singapore is projected to join other countries such as Japan and South Korea in becoming a super-aged society, where at least 21 per cent of the population are aged 65 or older.
ST PHOTO: GIN TAY
Currently, 20.7 per cent of Singaporeans are already in this group, up from 13.1 per cent in 2015. By 2030, about a quarter of all Singaporeans will be at least 65 years old.
To meet the needs of its rapidly ageing population, Singapore has been enhancing and diversifying measures to care for seniors.
In 2026, 200 community care apartments – which integrate senior-friendly housing with care services – will be launched near Caldecott MRT station in Toa Payoh, where about a quarter of residents are at least 65 years old.
From early 2026, an enhanced Home Personal Care service will be rolled out islandwide, offering greater support for seniors who choose to live in their own home, as well as tech-enabled monitoring and response for falls and other incidents.
The first quarter of 2026 will also see
the launch of the $260 million Perennial Living project
, Singapore’s first private assisted living development for seniors, which includes 200 suites, 100 nursing home beds and a 1.5ha therapeutic park.
In August 2025, the
Age Well Neighbourhoods initiative was announced
, which provides seniors with convenient access to social activities and healthcare in their neighbourhood, beginning with Toa Payoh and other areas with a higher concentration of seniors.
From April 1, new Integrated Shield Plan (IP) riders will
not be allowed to cover minimum deductibles patients have to pay before insurance kicks in
.
The annual co-payment cap will also be doubled from $3,000 to $6,000, meaning IP holders with the new riders will also need to pay a larger portion of their bills.
IPs provide optional health coverage by private insurers on top of national insurance scheme MediShield Life, which covers all Singaporeans, while riders are sold to cover the deductible as well as the remainder of the bill not covered by MediShield Life and IPs.
The changes are aimed at addressing rising insurance premiums and private healthcare costs.
They come on the back of six private insurers increasing premiums for most IPs or riders in 2025, citing pressures from rising claims, medical inflation and expanded benefits.
The Ministry of Health (MOH) estimates that premiums for the new riders will be about 30 per cent lower than those of existing ones with maximum coverage.
Only two of the 28 currently available plans can continue to be sold to new policyholders from April.
From Jan 1, national long-term care insurance scheme CareShield Life will offer
higher monthly cash payouts to help those with severe disabilities meet the rising costs of long-term care
.
The monthly payouts will grow at a rate of 4 per cent a year, compared with 2 per cent previously.
While premiums for the scheme will rise, the Government said it will provide an additional $570 million in premium support over the next five years to mitigate the impact of these hikes on policyholders.
In order to keep premiums in check, older individuals with mild and moderate disabilities can no longer opt in to the scheme from 2026.
Introduced in 2020 to replace ElderShield, CareShield Life provides lifelong monthly payouts for severe disability.
As part of preventive care initiative Healthier SG, general practitioners (GPs) will start to manage mild to moderate cases of anxiety and depression in the community from 2026.
This means that social service agencies can refer patients determined to have moderate mental health needs to a GP, rather than the Institute of Mental Health.
As at end-2024, more than 520 GPs had joined the Mental Health General Practitioner Partnership, supporting doctors in identifying, diagnosing and managing patients with mild to moderate mental health conditions.
GPs on the programme, which began in 2012, gain access to lower-cost psychiatric medicine as well as support from hospital-based psychiatrist-led teams.
Senior Minister of State for Health Koh Poh Koon said in July 2025 that
acute psychiatry services will be expanded across all healthcare clusters islandwide to enhance access to mental health care
.
The first statutory board to be launched in six years, the Communicable Diseases Agency (CDA) brings together public health functions for the detection, prevention and control of infectious diseases.
These capabilities previously came under MOH – CDA’s parent ministry – as well as the National Centre for Infectious Diseases (NCID) and the Health Promotion Board.
Speaking at CDA’s official launch in November, Prime Minister Lawrence Wong said
the new agency will lead efforts to refresh and update Singapore’s pandemic preparedness plans
.
In July 2025, CDA introduced the Singapore pandemic preparedness and response framework, which emphasises a flexible response to tackling both familiar and unknown disease threats.
Established in April 2025, CDA is chaired by Director-General of Health Kenneth Mak, with Professor Vernon Lee, formerly executive director of NCID, as the agency’s chief executive officer.
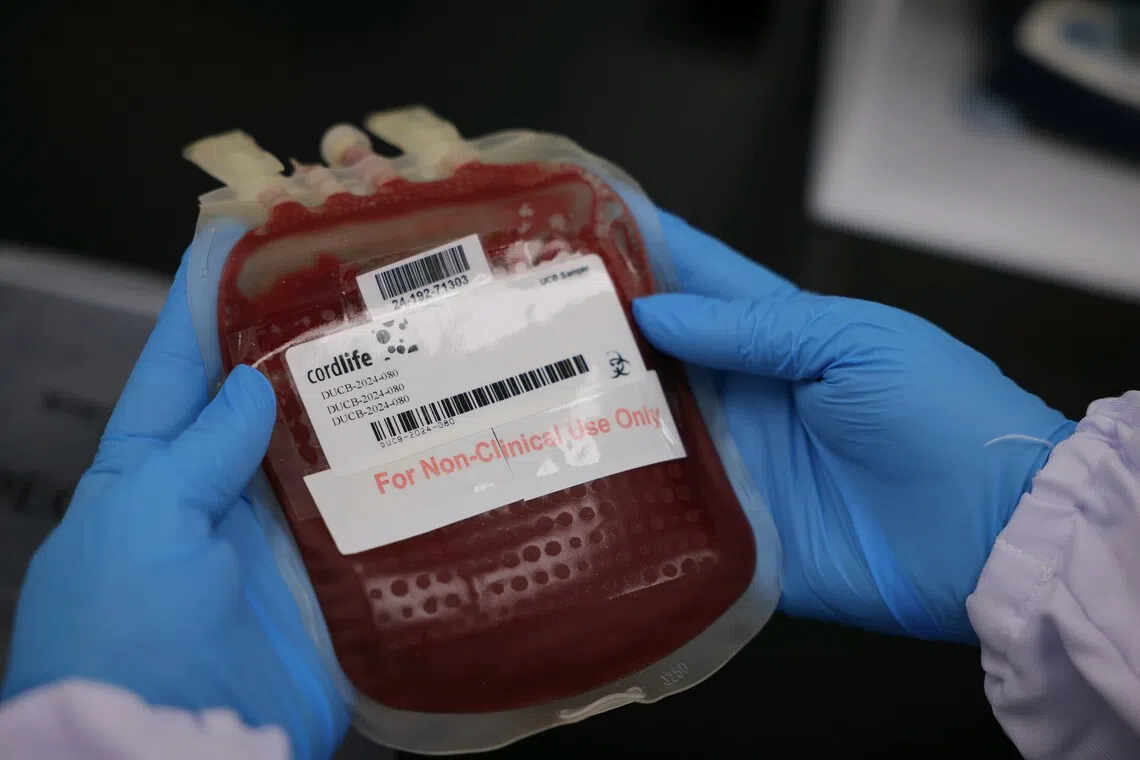
A lab technician holding cord blood in a demonstration of their process at Cordlife, on Sept 17, 2024.
PHOTO: ST FILE
Since November, private cord blood bank Cordlife has not been allowed to
collect, test, process and/or store new cord blood
.
The company can only maintain the storage of existing cord blood units, and perform actions such as facilitating their transfer to other cord blood banks and disposing of existing units if instructed to do so by clients.
These restrictions will remain in place even if Cordlife’s licence is renewed for a year in January, and until it demonstrates that it is able to consistently meet the regulatory requirements for its cord blood banking services.
This comes after MOH issued a notice to Cordlife in September that the ministry intended to suspend the company’s licence.
After considering its representations, the ministry said in November that Cordlife had not adequately addressed concerns raised during an audit.
These included failing to comply with regulatory requirements such as governance, incident reporting and management, as well as processes for collection, testing and processing of new cord blood units.
In December, The Straits Times reported that Cordlife is facing civil claims of at least $5.45 million from parents who had stored cord blood with the bank.

In November, Singapore’s largest polyclinic, Serangoon Polyclinic, opened its doors to the public.
ST PHOTO: AZMI ATHNI
In November,
Singapore’s largest polyclinic, Serangoon Polyclinic, opened its doors to the public
.
The seven-storey, 11,600 sq m facility is designed to serve the growing population of seniors in Serangoon, where about one in five residents is aged 65 or above.
Located across from Nex shopping mall and Serangoon MRT station, the polyclinic is expected to see about 1,300 patients each day.
The opening of Serangoon Polyclinic puts Singapore on track to have 32 polyclinics by 2030, up from 27 currently. Two polyclinics, Tengah and Kaki Bukit, are expected to be completed by 2026.
November also saw the launch of St Andrew’s Community Hospital (Bedok) – the Republic’s 11th community hospital and St Andrew’s second such facility – which supports Changi General Hospital in meeting healthcare needs in the eastern part of Singapore.
And in October, Alexandra Hospital began receiving ambulance cases as part of efforts to ramp up its emergency response ahead of developing a fully functioning emergency department in 2028, when it is redeveloped into an integrated health campus.
These developments come in anticipation of an increased demand for healthcare services as Singapore’s population rapidly ages.
In December, Health Minister Ong Ye Kung launched the Healthcare Facility Design Standards – a framework which harmonises hospital design principles across the public healthcare system – which could lead to new hospitals being built faster and at potentially lower costs.

